What it is like to have BPD
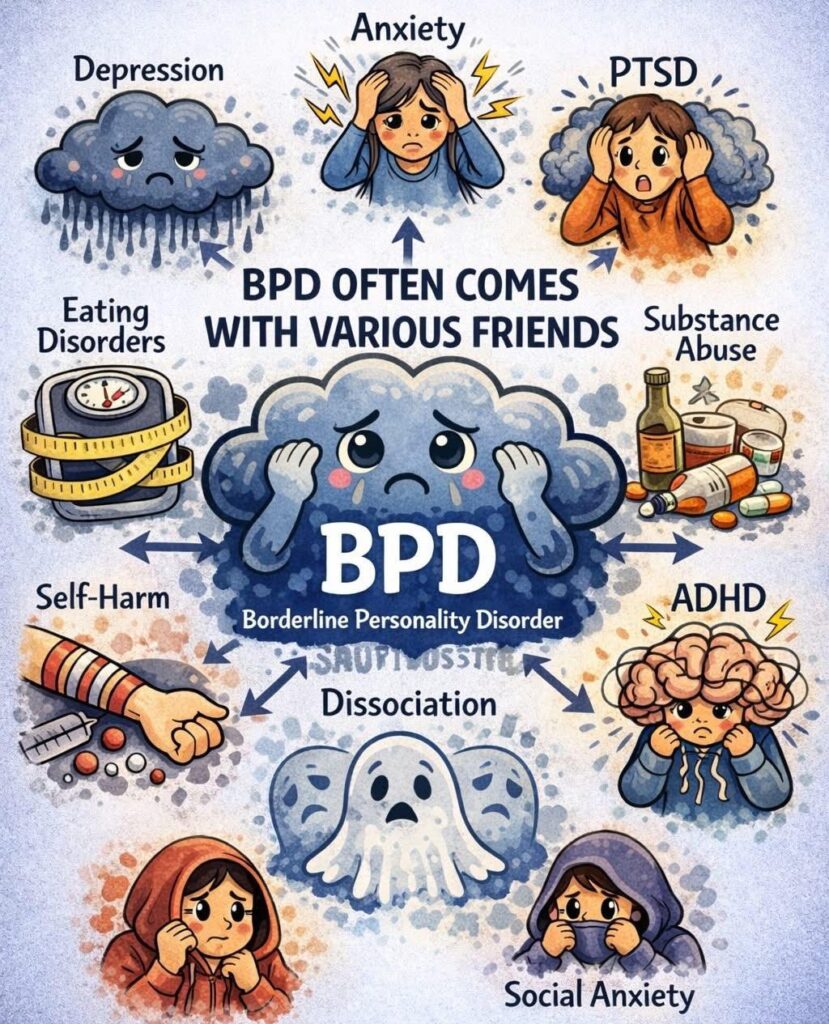
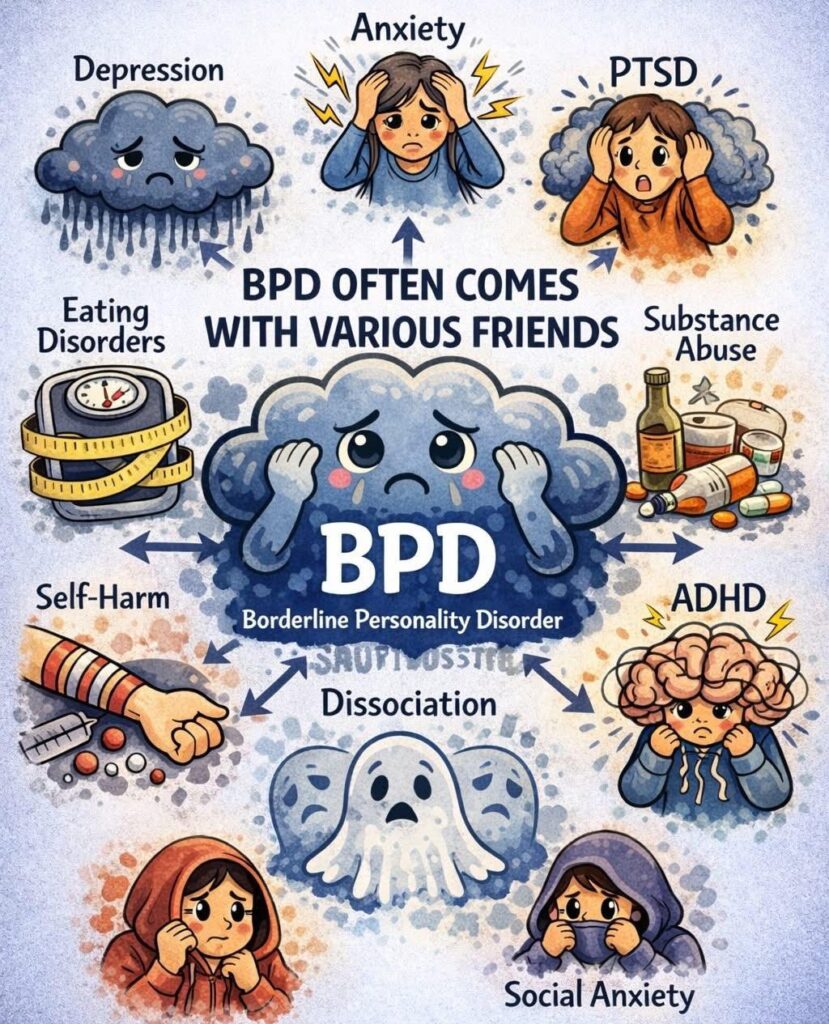
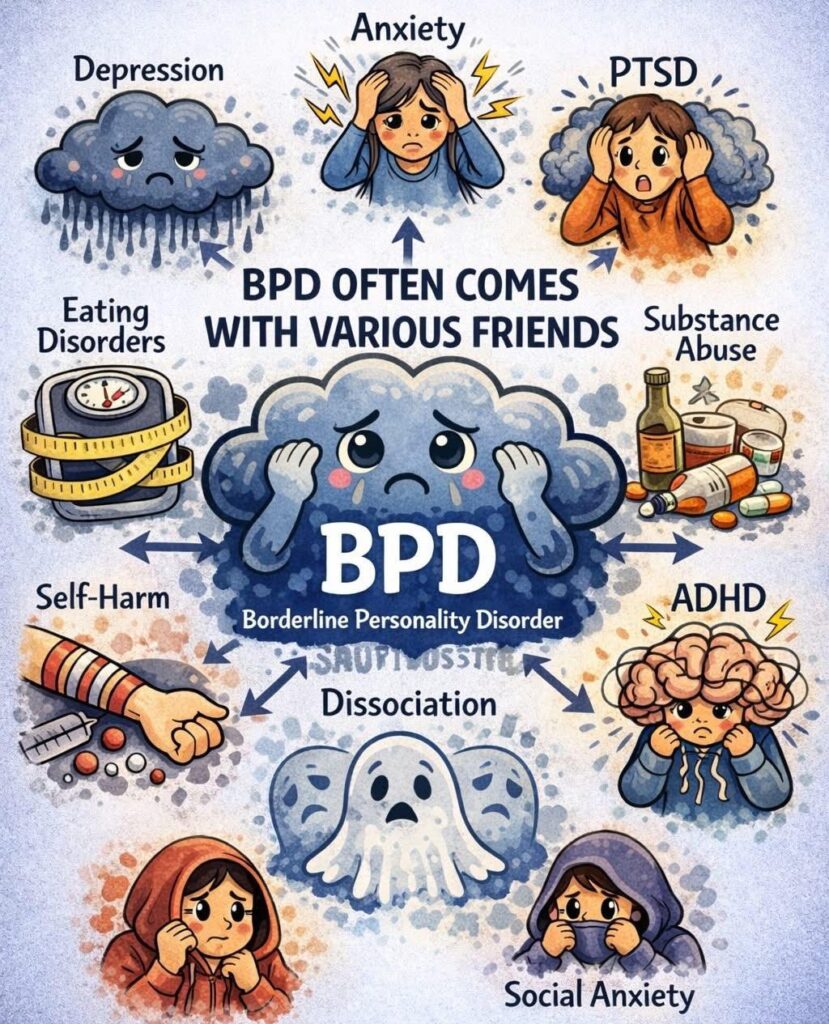
Borderline Personality Disorder (BPD) is a complex mental health condition characterized by pervasive instability in moods, behavior, self-image, and functioning. The diagnosis of BPD is typically based on a comprehensive clinical assessment that includes a detailed patient history and a mental status examination. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides the criteria for diagnosing BPD. According to the DSM-5, a diagnosis of BPD is made if there is a pervasive pattern of instability in interpersonal relationships, self-image, and affects, as well as marked impulsivity, beginning by early adulthood and present in a variety of contexts. This pattern is indicated by at least five (or more) of the following nine criteria:
Diagnosing BPD requires a comprehensive and nuanced approach, considering the patient’s history, symptom presentation, and the impact of symptoms on their daily life. A thorough assessment by a qualified mental health professional is essential for an accurate diagnosis and the development of an effective treatment plan. Treatment for BPD often includes psychotherapy, such as Dialectical Behavior Therapy (DBT), and may also involve medications to manage specific symptoms or comorbid conditions.
Cognitive behavioral therapy (CBT) is a type of psychotherapy that focuses on changing the way you think and behave. It is a well-researched and effective treatment for a variety of mental health conditions, including borderline personality disorder (BPD).
CBT for BPD can help you to:
CBT is typically offered in a group or individual setting. In group therapy, you will meet with other people who are also struggling with BPD. Together, you will learn about CBT and how to apply it to your own life. In individual therapy, you will work with a therapist to develop a customized treatment plan for you.
CBT for BPD is not a quick fix. It takes time and effort to learn and apply the skills you will need to manage your BPD. However, with hard work and dedication, CBT can help you to live a more fulfilling and satisfying life.
If you are interested in learning more about CBT for BPD, talk to your doctor or therapist. They can help you to find a therapist who is trained in CBT and who can help you to develop a treatment plan that is right for you.
Here are some of the benefits of using CBT for BPD:
If you are struggling with BPD, CBT can be a helpful treatment option. Talk to your doctor or therapist to find out more about CBT and to see if it is right for you.
Dialectical Behavior Therapy (DBT) is a form of psychotherapy that was originally developed by Marsha M. Linehan in the 1980s to treat individuals with Borderline Personality Disorder (BPD). Since then, it has been adapted to treat other mental health conditions such as depression, anxiety, eating disorders, substance abuse, and post-traumatic stress disorder (PTSD). DBT is a type of cognitive-behavioral therapy that combines elements of mindfulness, acceptance, and change strategies.
The theory behind DBT is that individuals who struggle with emotional regulation have an intense sensitivity to emotional stimuli, and a slower return to baseline levels of emotional arousal. This leads to a greater likelihood of impulsive behavior and difficulty regulating emotions, which can lead to problematic behaviors such as self-harm, substance abuse, and suicidal ideation. The goal of DBT is to help individuals learn skills to manage their emotions more effectively, increase their ability to tolerate distress, and reduce problematic behaviors.
DBT is based on four key components: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
Mindfulness is a practice that involves paying attention to the present moment without judgment. It is designed to increase awareness of one’s thoughts, emotions, and physical sensations. In DBT, mindfulness techniques are used to help individuals become more aware of their emotions and learn to observe them without reacting impulsively. Mindfulness is also used to help individuals become more present in their daily lives and reduce distractions that can lead to impulsive behavior.
Distress tolerance is the ability to tolerate and survive intense emotional experiences without engaging in problematic behavior. DBT teaches individuals specific techniques to manage distress, such as distraction, self-soothing, and physical activity. The goal of distress tolerance is to help individuals build up their emotional resilience and learn to manage difficult emotions in healthy ways.
Emotion regulation is the process of learning how to identify, express, and modulate emotions. DBT helps individuals learn to identify their emotional triggers, understand the function of their emotions, and develop strategies to regulate their emotions effectively. This includes skills such as problem-solving, self-soothing, and increasing positive experiences.
Interpersonal effectiveness focuses on developing skills to communicate effectively with others and establish healthy boundaries in relationships. DBT teaches individuals how to express their needs, say no, and negotiate effectively with others. It also helps individuals learn to navigate difficult interpersonal situations and reduce conflicts in their relationships.
DBT is typically delivered in a group format, with individual therapy sessions provided as needed. The group format allows individuals to receive support and feedback from others who are going through similar experiences. It also allows individuals to practice their new skills in a safe and supportive environment.
DBT has been shown to be an effective treatment for a variety of mental health conditions. Studies have shown that DBT is effective in reducing suicidal ideation and self-harm behaviors in individuals with BPD. It has also been shown to be effective in reducing symptoms of depression, anxiety, and substance abuse in individuals with co-occurring mental health conditions.
DBT is not a quick fix, and it requires a commitment to ongoing treatment. However, the skills learned in DBT can be life-changing for individuals struggling with emotional regulation and problematic behaviors. DBT has been shown to reduce hospitalizations, emergency room visits, and other costly forms of treatment.
In conclusion, DBT is a highly effective form of psychotherapy that has helped many individuals struggling with emotional regulation and problematic behaviors. It combines elements of mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness to help individuals learn skills to manage their emotions more effectively, increase their ability to tolerate distress, and reduce problematic behaviors.
In this proud land we grew up strong
We were wanted all along
I was taught to fight, taught to win
I never thought I could fail
No fight left or so it seems
I am a man whose dreams have all deserted
I’ve changed my face, I’ve changed my name
But no one wants you when you lose
Don’t give up
’cause you have friends
Don’t give up
You’re not beaten yet
Don’t give up
I know you can make it good
Though I saw it all around
Never thought I could be affected
Thought that we’d be the last to go
It is so strange the way things turn
Drove the night toward my home
The place that I was born, on the lakeside
As daylight broke, I saw the earth
The trees had burned down to the ground
Don’t give up
You still have us
Don’t give up
We don’t need much of anything
Don’t give up
’cause somewhere there’s a place
Where we belong
Rest your head
You worry too much
It’s going to be alright
When times get rough
You can fall back on us
Don’t give up
Please don’t give up
‘got to walk out of here
I can’t take anymore
Going to stand on that bridge
Keep my eyes down below
Whatever may come
And whatever may go
That river’s flowing
That river’s flowing
Moved on to another town
Tried hard to settle down
For every job, so many men
So many men no-one needs
Don’t give up
’cause you have friends
Don’t give up
You’re not the only one
Don’t give up
No reason to be ashamed
Don’t give up
You still have us
Don’t give up now
We’re proud of who you are
Don’t give up
You know it’s never been easy
Don’t give up
’cause I believe there’s the a place
There’s a place where we belong
https://www.eggshelltherapy.com/high-functioning-bpd
I can totally relate to this article. I am high functioning on the surface but deep turmoil underneath.
How about all of them?
https://themighty.com/2019/08/borderline-personality-disorder-bpd-types/
https://www.cnn.com/2019/03/05/health/esketamine-depression-nasal-spray-fda-bn/index.html
Could be very useful in dealing with the depression aspect of BPD, but the cost is going to be out of reach for most people.
When every thing seems just too much to deal with, and you are just overwhelmed by everything, remember the T.I.P. skills.
Fill a bowl with ice cold water. Hold you breathe and dunk your face into the water. Hold it there for as long as you can. The shock of the cold will activate the bodies ‘dive’ response. No bowl of cold water handy? Get some ice cubes and hold them in your hand, and if you can’t get ice cubes, try holding an ice cold drink, anything cold will help. The temperature change will slow down your heart rate and increase the flow of blood to the brain. This will help to lower the strength of the emotion.
Do something active! Run like crazy, dance, jog for a few minutes. This will expend the bodies energy and calm you down. Any intense exercise will do. Just try it next time.
Tense all your muscles at once, while you breathe in, then relax the muscles are breathe out, saying a word that will help you, like ‘Relax’, or ‘Peace’. You choose the word that works best for you.